Incision and drainage: indications and how to perform with photos
If the overlying skin is ischaemic or necrotic, or needle aspiration has failed, proceed to formal incision + drainage
Importantly, there's no reason to cease breastfeeding once abscess is diagnosed. Women can be reassured that milk leaking from an abscess incision site helps rather than hinders healing, due to its immunoprotective properties.
An abscess may grow in size or be located superficially. This causes tension on the skin, mechanically impacting upon the dermal vasculature. The perfusion of the skin overlying the abscess is then compromised and the skin appears dusky or necrotic. In this case, an incision into the skin and removal of the necrotic skin, typically in an operating theatre, facilitates resolution of ongoing inflammation and infection.1
Formal incision + drainage (I+D) is recommended if
-
The overlying skin is compromised, or
-
There is failure of resolution with directed antibiotic therapy (in response to microscopy, culture and sensitivites) and repeated needle aspirations.
I+D can be performed either in the outpatient setting or in theatre, depending on the skin status and size of the abscess. If the skin is viable, a small incision can be made to allow access to the abscess cavity. However, any necrotic tissue needs to be excised.
-
Some breast surgeons preference I+D over needle aspiration, proposing that I+D in their rooms without general anaesthesia using a stab incision and small ‘penrose’ drain allows for passive decompression of a lactational abscess and can be removed 1-4 days after the procedure, with drainage site closure occuring about 7 days post-procedure. A video of incision technique of an abscess or galactocoele is available here (Dr Katrina Mitchell).
-
However, many breast surgeons are concerned that I+D in their rooms with sedation and topical anaesthetic is too painful for the patient, depending on the clinical presentation, because of the limitations of local anaesthetic when incising and draining multi-located abscesses. When concerns about pain are raised, many women elect for I+D in the operating theatre.
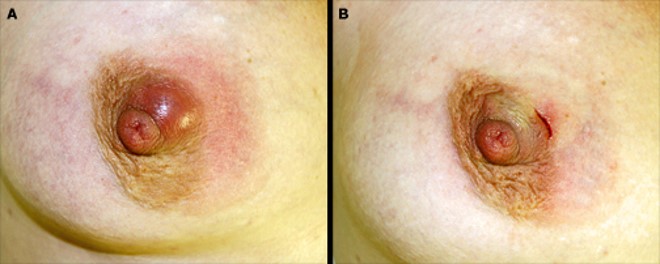
Images 1 and 2 show compromised skin overlying a lactational abscess, requiring incision and drainage.
Image 1

Image 2

How to conduct I+D on a breast abscess
-
Large incisions, drains or packing have not been shown to improve rates of abscess resolution, but have negative outcomes on patient cosmesis and satisfaction. The size of the incision does not have to be drastic. The purpose of the incision is to facilitate entry into the cavity, to break down loculations, and facilitate thorough drainage and irrigation. Over-sized incisions are cosmetically unappealing and unwarranted. However if the overlying skin is necrotic and needs to be debrided that is a different situation – that is when an abscess has led to a carbuncle formation.
-
The cavity is irrigated with local anaesthetic and adrenaline (using the same principles used in needle aspiration, here)
-
The stent is packed with gauze into a bra, allowing women to continue to breastfeed. Women can be reassured that milk leaking from the abscess incision site helps rather than hinders healing, due to its immunoprotective properties.
-
Repeat ultrasound imaging is required after incision and drainage.1, 2
Image 3

Image 4

Image 5
Acknowledgements
The breastfeeding art on this page is purchased from, and kindly used with consent by, Camilla Kleist at www.kleist-art.me.
Images 1 and 2: Scott 2022
Images 3-5: Dixon & Kahn 2011
References
-
Eryilmaz R, Sahin M, Hakan Tekelioglu M, Daldal E. Management of lactational breast abscesses. Breast. 2005 Oct;14(5):375-9.
-
Scott DM. Inflammatory diseases of the breast. Best Pract Res Clin Obstet Gynaecol. 2022 Sep;83:72-87. doi: 10.1016/j.bpobgyn.2021.11.013.
-
Dixon JM, Khan LR. Treatment of breast infection. BMJ 2011; 342:d396.
