ABM Clinical Protocol #36's distinction between inflammatory vs bacterial mastitis is unhelpful and promotes overuse of antibiotics
Inflammatory and bacterial mastitis are redundant diagnoses
The Academy of Breastfeeding Medicine's Clinical Protocol #36 creates two new diagnoses for 'mastitis'. Here is why these diagnoses are unhelpful and risk unintended outcomes.
Mastitis means 'inflammation of the breast'. All mastitis is inflammatory.
-
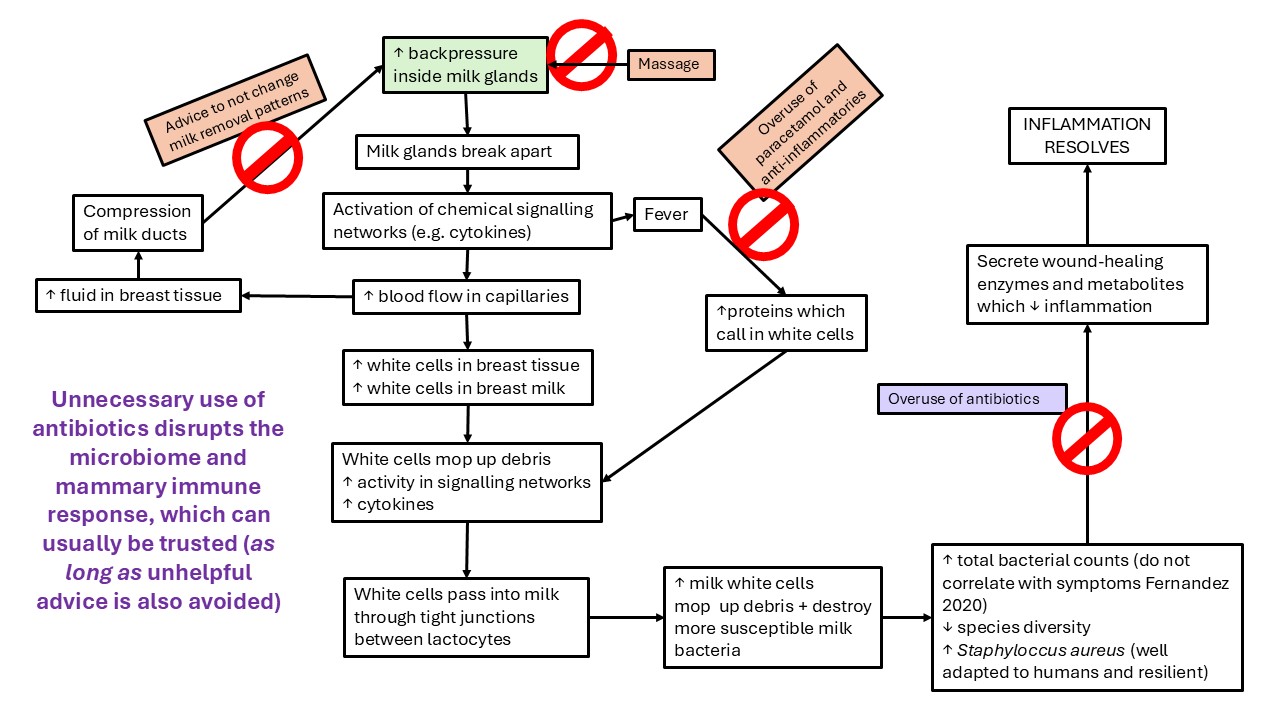
Because all mastitis is inflammatory, the diagnosis 'inflammatory mastitis' is a tautology and not meaningful. Even more severe presentations on the spectrum of mastitis are associated with systemic signs and symptoms which do not necessarily correlate with need for antibiotics.
-
All mastitis or breast inflammation affects both breast milk and stroma, as the mammary immune system acts to respond to and to downregulate the inflammation. All mastitis will be associated with altered bacterial populations and increased counts of hardier bacteria in the milk microbiome, which is demonstrated in the research, as a result of elevated leucocyte and other activity. The same alteration is likely in the sparse but documented breast stromal microbiome (though that theory has not been researched).
Clinical Protocol #36 uses a fever of longer than 24 hours duration to define a progression from ‘inflammatory mastitis’ to ‘bacterial mastitis’, and cannot otherwise accurately distinguish between the two. (The sign of tachycardia is inevitably associated with fever.) This difficulty in defining the difference is because mastitis is a spectrum condition - and it doesn't make sense to both apply the concept of a spectrum condition and then nevertheless attempt to engage hard definitions. Clinical Protocol #36 also suggests that the efficacy of probiotics and antibiotics is diagnostic.
Clinical Protocol #36 states:
“Inflammatory mastitis presents as an increasingly erythematous, edematous, and painful region of the breast with systemic signs and symptoms such as fever, chills, and tachycardia.”
“Bacterial mastitis represents a progression from ductal narrowing and inflammatory mastitis to an entity necessitating antibiotics or probiotics to resolve … Bacterial mastitis presents as cellulitis (worsening erythema and induration) in a specific region of the breast that may spread to different quadrants … An evaluation by a medical professional should be performed if there are persistent systemic symptoms (>24 hours) such as fever and tachycardia … In the absence of systemic signs and symptoms, diagnosis should be considered if the breast is not responding to conservative measures described … Reserve antibiotics for bacterial mastitis …”
Cellulitis is not a feature of lactation-related mastitis
Mastitis is typically associated with involvement of the overlying skin in the inflammatory cascades, with vasodilation and erythema. This is
-
Secondary, specifically related to skin overlying the lump
-
Quite distinct from a primary infective cellulitis, which is a spreading bacterial infection of the skin alone.
Cellulitis is not a usual feature of lactation-related mastitis, and requires antibiotics if it is progressing rapidly or severe.
A fever that persists for longer than 24 hours does not necessarily require a visit to the doctor and does not indicate a diagnosis of 'bacterial mastitis' nor antibiotics
The advice to visit the doctor if fever has persisted for longer than 24 hours to assess for bacterial mastitis promotes unnecessary visits to the doctor, and is likely to promote unnecessary use of antibiotics. Mastitis often takes much longer to resolve than 24 hours, though it usually resolves without antibiotics, and mastitis is commonly associated with fever.
Kvist et al (2006, 2007, 2008) showed that early use of antibiotics does not improve outcomes or protect against abscess formation. Kvist also showed that even with fever, most breast inflammations resolved with conservative measures, including fit and hold intervention and increased frequency of feeds. The team also showed that occurrence of fever didn't predict the length of the illness.
Recommended resources
Mastitis management: secondary outcomes, indication for antibiotics, prevention
Selected references
-
Douglas PS. Re-thinking benign inflammation of the lactating breast: classification, prevention, and management. Women's Health. 2022;18:17455057221091349.
-
Douglas PS. Does the Academy of Breastfeeding Medicine Clinical Protocol #36 'The Mastitis Spectrum' promote overtreatment and risk worsened outcomes for breastfeeding families? Commentary. International Breastfeeding Journal. 2023;18:Article no. 51 https://doi.org/10.1186/s13006-13023-00588-13008.
-
Kvist LJ, Hall-Lord ML, Rydhstroem H, Larsson WB. A randomised-controlled trial in Sweden of acupuncture and care interventions for the relief of inflammatory symptoms of the breast during lactation. Midwifery. 2006;23(2):184-195.
-
Kvist LJ, Halll-Lord ML, Larsson BW. A descriptive study of Swedish women with symptoms of breast inflammation during lactation and their perceptions of the quality of care given at a breastfeeding clinic. International Breastfeeding Journal. 2007;2:2.
-
Kvist L, Larsson BW, Hall-Lord ML, Steen A, Schalen C. The role of bacteria in lactational mastitis and some considerations of the use of antibiotic treatment. International Breastfeeding Journal. 2008;3:6.
-
Kvist LJ. Toward a clarfication of the concept of mastitis as used in empirical studies of breast inflammation during lactation. Journal of Human Lactation. 2010;26(1):doi:10.1177/0890334409349806.
-
Kvist L. Diagnostic methods for mastitis in cows are not appropriate for use in humans: commentary. International Breastfeeding Journal. 2016;11(2):doi 10.1186/s13006-13016-10061-13001.
