Fine needle aspiration: indications and how to perform (PAIR method) with photos and demonstration video
Start here if skin overlying the abscess is healthy: needle aspiration + irrigation
Importantly, there's no reason to cease breastfeeding when an abscess is diagnosed. Women can be reassured that any milk which might occasionally leak from an abscess fine needle aspiration site immediately after the procedure helps rather than hinders healing, due to its immunoprotective properties.
If the skin overlying a lactational abscess is healthy, needle aspiration (NA) (by the PAIR method) is indicated.1-6 You can view Dr Ofri (Breast Surgeon) demonstrating this at the bottom of the page.
Rates of resolution after a single aspiration are between 47-64%, with an overall NA success rate of 75-96%. When compared to incision and drainage (I+D), patients have
-
Less pain
-
A shorter healing time
-
Less ductal damage and fistula risk and
-
Better cosmetic outcome.
Over 90% patients that are needle aspirated typically continue breastfeeding, compared to 29% of those who undergo I+D, most likely due to the mother being separated from the baby or due to surgeon recommendation.
A 2023 meta-analysis by Zhou et al, which selected 9 randomised controlled trials, concluded:
Needle aspiration (NA) has better advantages in terms of healing time, avoidance of breast fistula, continuous breastfeeding, and patient satisfaction. Although NA and ID have similar cure and recurrence rates, NA, with or without ultrasound guidance, could be used as a first-line treatment for breast abscesses. Patients with large volumes, multicompartmental abscesses, or those who have been ineffective against multiple NA, should be considered for ID. 5
In a 2019 study by Colin et al in France, the surgeons performed needle aspiration on 92 consecutive women with 105 lactational abscesses, without necrotic overlying skin. The median diameter of the abscess was 4.5cm with 40 of the 105 abscesses (38%) over 5 cm in diameter.
-
The maximum number of aspirations required were 6, with 4 patients who failed and required incision and drainage (I+D) (general anaesthetic and surgery).
-
In 47% of patients, a single aspiration was required for resolution.
-
2 punctures for 31%
-
3 punctures for 8%
-
And 4 or more covered 14%.
-
-
86% of patients resolved after 3 or less needle aspirations (that is, using bedside needle techniques).4
How to perform needle aspiration (PAIR method)
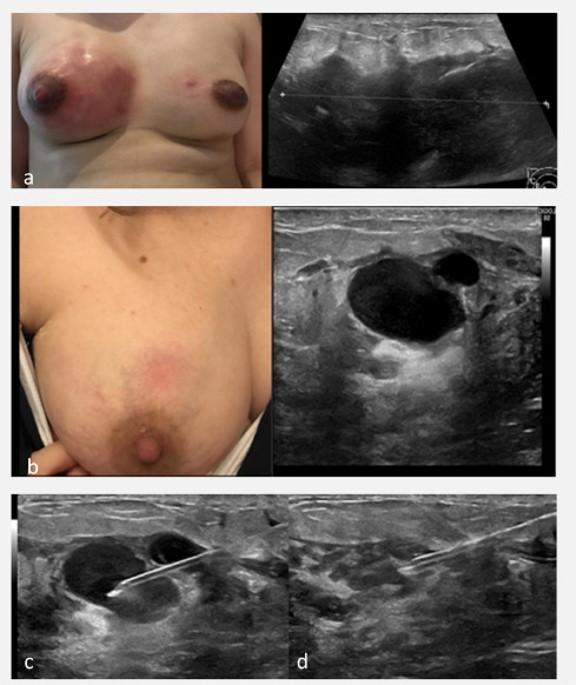
Images 1-3 below demonstrate needle aspiration of an abscess.
Performing NA under ultrasound guidance allows visualisation of any loculated areas and facilitates maximal drainage. However, you may have heard of the PAIR technique for hydatid cysts, denoting
-
Puncture (P)
-
Aspiration (A)
-
Instillation (I)
-
Re-aspiration (R).
This same acronym aapplies to needle aspiration for lactational abscess.4,5 The cavity is irrigated with a local anaesthetic solution. "The solution to pollution is dilution" is a classic surgical adage. Continually irrigating a wound decreases the bacterial load.
In this situation the benefit of irrigation is that it
-
Facilitates further break down of collections
-
Softens purulent debris to facilitate aspiration
-
Irrigates and removes any residual bacterial load that remains post-aspiration.
-
Local anaesthetic reduces the pain associated with the abscess.
Typically adrenaline is used because it can help with vasoconstriction, but to date there is no evidence that has shown adrenaline's benefits.
If we presume the typically size of a breast abscess that requires drainage is 30mm, we can calculate that roughly the volume of that cavity is 15ml to approximately 20ml (basing it off the volume of a sphere being 4/3 x pi x r^3). Subsequently irrigation with 40ml seems to be a good amount, but in practice we want to irrigate until it appears clear and no gross contamination is present.
When performing aspiration, irrigation has been shown to improve outcomes. This is best performed under ultrasound guidance to ensure adequate irrigation. Be aware that injecting excessive volume can result in discomfort and pain to the patient. Typical irrigation involves
-
Instillation of up to 40 ml of 1% lidocaine with adrenaline into the abscess cavity
-
Continuing with irrigation and aspiration until there is a clear return, and
-
The cavity has collapsed, if using ultrasound, or
-
The aspiration is dry.
-
-
Repeat this process every two or three days until complete resolution of the abscess (i.e. there is no further pus or fluid in the cavity on aspiration).
The first aspiration of purulent debris should be sent for microscopy, culture and sensitivies (MCS) to guide antibiotic therapy.
Progression to formal incision and drainage (I+D) is required if needle aspiration + irrigation have failed. Failure of resolution with NA is more likely to occur
-
In multiloculated abscess or
-
An abscess > 5cm in size.
Image 1

Image 2

Image 3
Video demonstration (simulated) of fine needle aspiration of a lactation-related abscess using the PAIR technique by Dr Adam Ofri (Breast surgeon)
Acknowledgements
The breastfeeding art on this page is purchased from, and kindly used with consent by, Camilla Kleist at www.kleist-art.me.
Images 1-3: Hu et al 2023
References
-
Pileri P, Sartani A, Mazzocco Mea. Management of breast abscess during breastfeeding. International Journal of Environmental Research and Public Health. 2021;19:5762.
-
Sazal HR, Haque N, Afroz C, Hasan S. Clinico-pathological profile and outcome of multiple ultrasonogram guided aspiration of breast abscess in outpatient department setup: a prospective study. Mymensingh Medical Journal. 2024;33(2):453-460.
-
Rigourda V, Benoitc L, Paugamb C. Management of lactating breast abscesses by ultrasound-guided needle aspiration and continuation of breastfeeding: a pilot study. Journal of Gynecoly Obstetrics and Human Reproduction 2022;51:102214.
-
Colin, C., et al., Breast abscesses in lactating women: evidences for ultrasound-guided percutaneous drainage to avoid surgery. Emergency Radiology, 2019. 26(5): p. 507-514.
-
Rigourd, V., et al., Management of lactating breast abscesses by ultrasound-guided needle aspiration and continuation of breastfeeding: A pilot study. Journal of Gynecology Obstetrics and Human Reproduction, 2022. 51(1): p. 102214.
-
Zhou F, Lia Z, Liua L. The effectiveness of needle aspiration versus traditional incision and drainage in the treatment of breast abscess: a meta-analysis. Annals of Medicine. 2023;55(1):2224045.
-
Hu Y, Li Y, Zou J, Xu Y. Indwelling Needle Puncture and Irrigation in the Conservative Treatment of Breast Abscess During Non-Lactation Period. J Vis Exp. 2023 Sep 22;(199).
