The milk-making glands inside your working breast
The glands (or alveoli)
Here, in the milk-making cells of our body, we see how 3.7 billion years of life on this planet has evolved into an extraordinarily sophisticated system connecting your little baby to your own immune system and your body's nutrients. In this breathtakingly complex biological system, your own precious body provides your baby's gut, brain, and developing tissues with myriad bespoke immune, metabolic and nutritional protections.
A single milk gland is known as an alveolus. Each alveolus secretes creates milk, and also holds that milk in the lumen for a while as it accumulates. There are thousands of these amazing little glands working hard in your breasts day and night once you start lactating. Each alveolus has an abundant capillary network wrapped around it, securing blood supply, carrying in the necessary nutrients and immune cells, and removing waste.
In the 2000's, ground-breaking ultrasound studies using high resolution ultrasound by Professor Donna Geddes from The University of Western Australia radically changed how we thought of the lactating breast. Her teams at the Geddes Hartmann Human Lactation Research Centre continue, year by year, to revolutionise international understandings of how the lactating breast works. She and her teams discovered that
-
Two-thirds of a lactating woman's glandular tissue is located in a radius of just 30mm from the base of her nipple
-
The amount of glandular tissue or number of ducts found in women who are exclusively and successfully breastfeeding doesn't relate to milk production and milk storage capacity. (Milk production is mostly controlled by how often your baby takes milk from your breast.)
-
A woman's two breasts usually have symmetrical proportions of glandular and fatty tissue, even though breasts are often asymmetrical in size in the one woman.
-
There is on average about twice as much glandular tissue as fatty tissue in a lactating breast. But this proportion varies a lot. Some lactating breasts are over 80% glandular tissue, other normal lactating breasts contain just 45% glandular tissue. There is no relationship discovered to date between the amount of glandular tissue and milk production.
Please scroll down to read about the three kinds of cells and basement membrane which make up an alveolus gland.
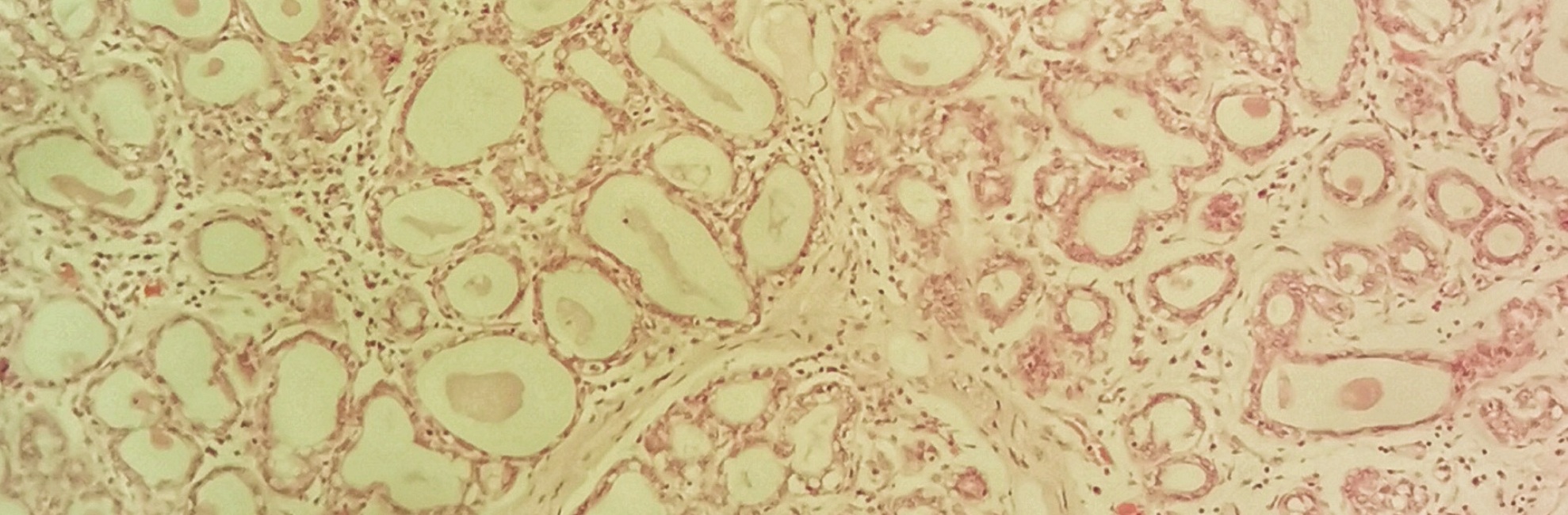
The image above shows mammary gland tissue prepared histologically, and magnified, so that you can see the alveoli with lumens full of milk, surrounded by lactocytes. They alveoli look like lots of irregularly shaped balloons! The lactocytes lining the alveoli in this tissue preparation are stretched out to thin rectangles because the alveoli are full.
1. Milk-making cells (or lactocytes)
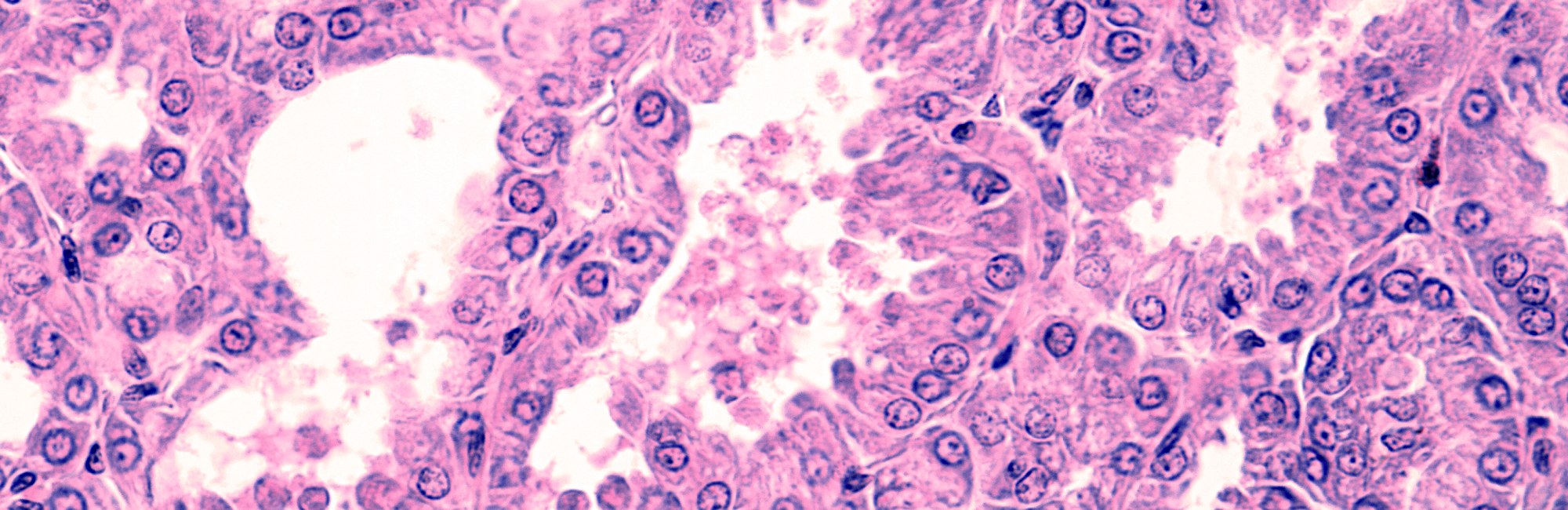
An alveolus is made up of three kinds of cells, found in two layers. The first layer are the milk-secreting cells known as lactocytes, which nestle together just one-cell deep around the gland's inner milk sac or lumen.
Lactocytes are a form of epithelial cell. They join together at ‘tight junctions’, formed when two lactocyte surfaces rest side by side touching each other. Tight junctions between the lactocytes open up quite easily. (Lactocyte tight junctions aren't tough and tight like the collagen joints which stick keratinocytes together in your nipple skin.)
-
Lactocytes constantly secrete milk into the alveolar lumens. A small amount of milk also flows out into and rests in the milk ducts, under the positive pressure of milk secretion within the alveoli.
-
When there isn't much milk in the lumen, the lactocytes take on a somewhat triangular shape, with their inside wall shaped into an apex or softly rounded point.
-
As the lumen expands more and more with milk, compression forces (which I’ll call back-pressure in the milk glands) causes sustained stretching of the lactocytes. They respond to this by changing shape. The apical projection into the lumen is compressed and disappears, so that the lactocyte elongates and its surface area is reduced. This helps protect the tight junctions, to prevent them from opening up and leaking - or breaking altogether.
2. The starlike contractile cells (or myoepithelial cells)
Each alveolus is wrapped in a network of starlike, branching cells, the myoepithelial cells, which contain lots of contractile protein, and are a kind of smooth muscle. Together, the lactocytes and the myoepithelial cells make up what's known as the mammary epithelium.
When your breast tissue is bathed in oxytocin, these myoepithelial cells press the milk out of those hundreds of thousands of little sacs into the ducts. You could say your oxytocin surge is like a great wine press, which gently treads the juice from the grapes, resulting in a let-down.
The size of the alveolar gland surface area decreases by about a third during a contraction, becoming randomly and irregularly squashed up. At any one time, the synthesis of milk is occurring at different rates across your breast. This means that some lumens even within the same lobule are much fuller than others. So the whole process of a milk let-down is not synchronised and machine-like, but a rippling irregular effect throughout the breast.
3. Stem cells
The alveolus is such a dynamic and generative environment that it turns cells over much quicker than most other tissues in the body. Tucked amongst both the lactocytes and the myoepithelial cells are various kinds of stem cells. These extraordinary cells contain the future. They wait until they receive the right chemical signal then blossom forth into the kind of tissue the alveolus needs: either new lactocytes, or new myoepithelial cells.
4. The basement membrane
A basement membrane wraps around each alveolus and each milk duct, separating it from the breast's connective tissue. The basement membrane is extremely dense, but only 0.2 micromillimetres thick.
Recommended resources
Working breasts are diverse on the outside
The size of your breasts doesn't predict how much milk you'll make
Working breasts are diverse on the inside
Selected references
Biswas SK, Banerjee S, Baker GW. The mammary gland: basic structure and molecular signaling during development. International Journal of Molecular Science. 2022;23(7):3883 doi: 3810.3390/ijms23073883. PMID: 35409243; PMCID: PMC28998991.
Cox DB, Kent JC, Casey TM, Owens RA, Hartmann PE. Breast growth and the urinary excretion of lactose during human pregnancy and early lactation: endocrine relationships. Experimental Physiology. 1999;84:421-43
Geddes DT. Ultrasound imaging of the lactating breast: methodology and application. International Breastfeeding Journal. 2009;4:doi:10.1186/1746-4358-1184-1184.
Geddes DT. Inside the lactating breast: the latest anatomic research. Journal of Midwifery and Women's Health. 2007;52(6):556-563.
Geddes DB. The anatomy of the lactating breast: latest research and clinical implications. Infant. 2007;3(2):59-61.
Geddes, D.T.; Aljazaf, K.M.; Kent, J.C.; Prime, D.K.; Spatz, D.L.; Garbin, C.P.; Lai, C.T.; Hartmann, P.E. Blood flow characteristics of the human lactating breast. J. Hum. Lact. 2012, 28, 145–152.
Gooding M, Finlay J, Shipley J. Journal of Ultrasound Medicine. 2010;29(1):95-103.
Mortazavi SN, Hassiotou F, Geddes DT, Hassanipour F. Mathematical modeling of mammary ducts in lactating human females. Journal of Biomechanical Engineering. 2015;137:071009-071001-071007.
Ramsay DT, Kent JC, Hartmann RA, Hartmann PE. Anatomy of the lactating human breast redefined with ultrasound imaging. Journal of Anatomy. 2005;206:525-534.
Ramsay DT, Kent JC, Owens RA, Hartmann PE. Ultrasound imaging of milk ejection in the breast of lactating women. Pediatics. 2004;113:361-367.
Stewart TA, Hughes K, Stevenson AJ, Marino N, Ju AL, Morehead M, et al. Mammary mechanobiology - investigating roles for mechanically activated ion channels in lactation and involution. Journal of Cell Science. 2021;134:doi:10.124/jcs.248849.
Thomas EC, Wlliams TM, Hartmann PE. Lactation and mother's milk: recent advances in understanding. Infant. 2010;6(3):86-90.
