Diagnosing persistent lactation-related nipple pain as chronic neuropathic pain, nociplastic pain, or central sensitisation is inaccurate and risks inappropriate treatments and their side-effects
Stabbing or radiating pain into the breast during lactation may be a form of acute nerve irritation or neuralgia due to mechanical forces acting upon nerves in the nipple stroma
NDC guidelines apply the mechanobiological model of nipple pain to propose that
-
In the context of acute nipple inflammation, with the associated hypervascularity and histamine and cytokine release, mechanical pressure (either breastfeeding, pumping, or pressure of water in the shower, bedsheets, or touch by an examiner using a cotton bud or pin prick) triggers nociceptive pain perception.
-
Peripheral nerve irritation may occur inside the nipple stroma when the nipple stroma is subjected to repetitive bending, tensile, or deformational forces. This can result in nerve pain - stabbing, radiating, unpredictable pain in the breast. This nerve pain might also be referred to as an acute neuropathic pain, or a neuralgia, which occurs in direct response to inflammation or compression (by interstitial pressures) of peripheral somatosensory nerves in the nipple core.
-
Acute local pain and sensitivity in response to touch may be described as allodynia or as peripheral sensitisation, according to the most recent International Association for the Study of Pain terminology, which acknowledges that skin inflammation may cause allodynia.
-
Local sensitivity effects of nipple and breast inflammation should not be confused with central sensitisation, chronic neuropathy, or nociplastic pain. Persistent nipple pain should not be treated with medications which are often prescribed for chronic neuropathies.
Persistent nipple pain doesn't fit the category of acute neuropathic pain
Quote Doshi et al 2021: "Implicit in almost all discussions of neuropathic pain is its characterization as a chronic pain disorder, yet commonly, chronic neuropathic pain begins as an acute pain state. Acute neuropathic pain presents a diagnostic challenge. Both the terms "acute pain" and "neuropathic pain" encompass broad, heterogeneous, loosely defined sets of conditions and pathologies."
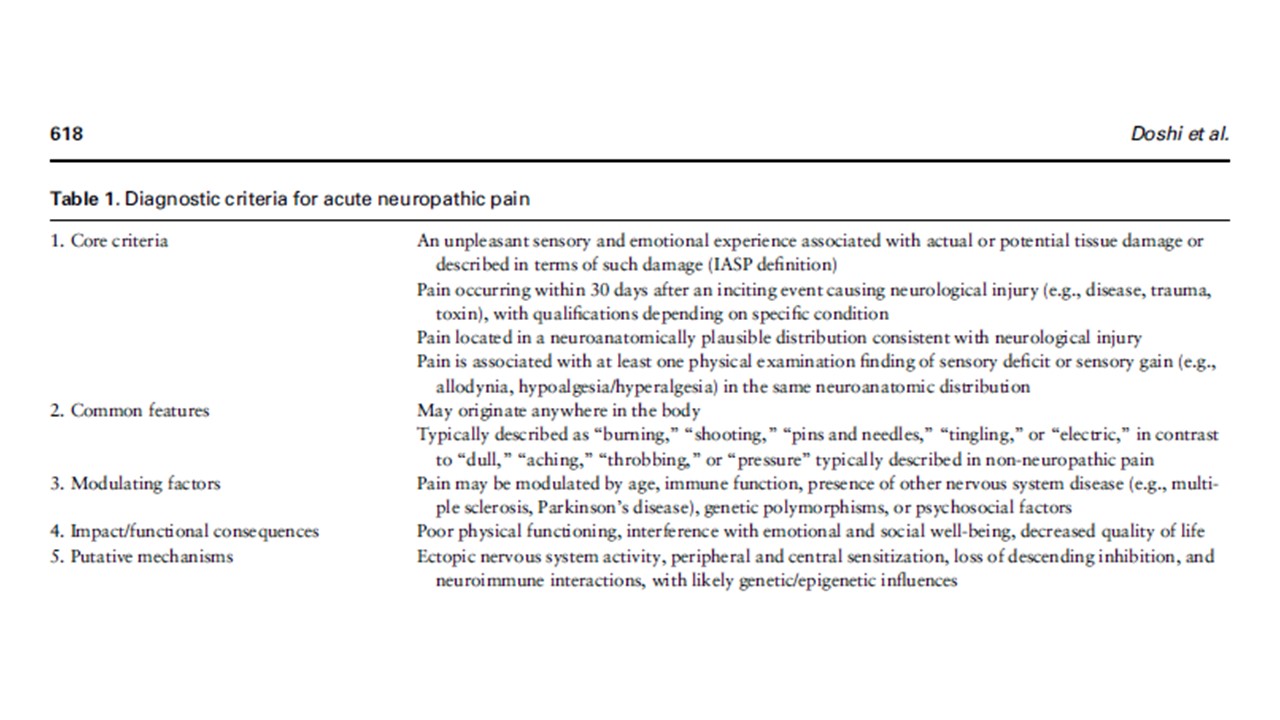
Table 1 from Doshi et al show the criteria for a diagnosis of acute neuropathic pain developed by a public-private partnership in the US, a working group which included the American Pain Society and the American Academy of Pain Medicine. You will see that the putative mechanisms for the diagnosis of acute neuropathic pain don't really appear apply to persistent nipple pain, because the nipple is being repeatedly subject to mechanical forces. Women variously describe their nipple and breast pain as burning, shooting, dull, electric, aching, and throbbing.
The diagnoses of neuropathic pain or central sensitisation are inappropriately applied to lactating and breastfeeding women experiencing persistent nipple pain
Some breastfeeding medicine health professionals apply the diagnoses of nociplastic pain, chronic neuropathic pain, or central sensitisation when a breastfeeding or lactating woman experiences persistent nipple pain. These definitions are not being applied in alignment with the International Association of Pain Study's definitions, discussed here.
Finnerup et al 2025
Neuropathic pain is defined by the International Association for the Study of Pain (ISAP) here.
Neuropathic pain is a lesion of the somatosensory system. Finnerup et all observe that the new IASP definition of neuropathic pain means that a condition like chronic regional pain syndrome is not considered a neuropathic pain syndrome because in chronic regional pain syndrome, the somatosensory system is intact. Neuropathic pain lacks robust classification or scoring systems, but is divided into three classes: possible, probable, and definite neuropathic pain.
-
Examples of peripheral neuropathic pain are postamputation pain, trigeminal neuralgia, painful radiculopathy, painful polyneuropathy, postherpetic neuralgia, peripheral nerve injury pain.
-
Examples of central neuropathic pain are central post-stroke pain, central pain in multiple sclerosis, spinal cord injury neuropathic pain.
Neuropathic pain is described as burning, tingling, or stinging and can be persistent even in the absence of visible tissue injury. The onset and progression of neuropathic pain has been linked to pro-imflammatory cytokines by numerous research studies. Numerous immune cells such as lymphocyctes, macrophages, dendritic cells, natural killer cells, mast cells, and stromal cells synthesise cytokines (which are soluble proteins). These proteins engage in the immune response. An extensive array of scientific investigations has repeatedly shown a strong relationship between high pro-inflammatory cytokine levels and neuropathic pain severity. The infection or nerve injury prompted excessive release of pro-inflammatory cytokines. That is, the immune system interacts with the nervous system in pain experience.
Zolezzi et al 2022
Not every chronic pain is neuropathic pain. For instance, chronic pain from arthritis results from a normal activation of pain pathways by inflammatory mediators surrounding a joint. Pain from a minor foot sprain would be considered normal and nociceptive because it is signaled by tissue injury (i.e., a normal mechanism).
Inflammatory pain from arthritis (center) is an example of a nociceptive mechanism because inflammation is the cause of pain. Inflammation is also pathophysiologic because it involves an altered (i.e., disease) state.
Neuropathic pain is considered only as pathophysiologic because pain is elicited by abnormal pain mechanisms. Normal pain is only acute, whereas inflammatory or neuropathic pain may be acute or chronic.
In most cases, neuropathic pain cannot be related to specific nerves or cortical areas, because neuroplastic changes occur beyond anatomy.
Pharmacotherapy for neuropathic pain targets specific action sites to achieve analgesic effects for different mechanisms of pain. However, when the mechanisms of pain for a patient are not characterized appropriately, pharmacotherapy may become inefficient. According to the latest review of the Canadian Pain Society Consensus statement, the pharmacological treatment for neuropathic pain are gabapentinoids (gabapentin and pregabalin), tricyclic antidepressants, and serotonin-norepinephrine reuptake inhibitors as first-line agents. Tramadol and opioids are second-line treatments, and cannabinoids have been moved from a fourth-line to a third-line treatment option (Mu et al., 2017).
The diagnoses of nociplastic pain, neuropathic pain, or central sensitisation may accidentally harm lactating women
Diagnoses of nociplastic pain, central sensitisation, neuropathic pain, and hyperalgesia may harm a lactating woman with nipple pain and damage. The International Association for the Study of Pain pain definitions are found here. This is because these diagnoses may
-
Invalidate her lived experience, which is that suckling or mechanical milk removal cause her pain and that if she were to cease this altogether, her pain would rapidly resolve;
-
Disempower her, since she is not helped to resolve the pain herself (as is the case, for example, with the gestalt method of fit and hold) but is informed she requires pharmaceutical intervention and multi-disciplinary teams;
-
Re-traumatise her if she is a sexual abuse survivor by taking a sexual trauma history in a breastfeeding consultation then proposing that persistent nipple pain is linked to sexual trauma and associated nociplastic effects;
-
Invite her to shift attention away from her experience of nipple pain. She may also feel pressured to divert her attention away from her nipple pain so that she is not perceived as ‘exaggerating’ the pain in her brain. Not paying attention to nipple sensations and pain typically worsens conflicting intra-oral vectors of force during milk removal. From the perspective of the gestalt method, increased attention to nipple and breast sensation is required, drawing on psychological strategies which support contact with the present moment, as she applies micromovements in order to eliminate breast tissue drag and resolve tissue damage and inflammation;
-
Place her at risk of side-effects of pharmaceutical interventions without evidence of benefit. For example,
-
SSRIs place some patients at risk of discontinuation or withdrawal syndrome, often misdiagnosed as an ongoing and long-term need for the SSRI.
-
Gabapentin may cause a low-grade headache.
-
-
Result in financial burden of treatments without evidence of benefit.
The research shows only modest or limited benefits from medications usually prescribed for chronic neuropathic pain (which is not lactation-related)
Quote from Zolezzi et al re treatment of chronic neuropathic pain (that is, neuropathic pain which has lasted three months or more): "Usually a combination therapy is preferred (Holbech et al., 2017) because of greater analgesic activity with mutual reinforcing effects of drugs, and better tolerability profile with reduced symptoms such as anxiety, depression and sleep disturbance (Gilron et al., 2013). There is some evidence showing that at least 45% of patients with neuropathic pain are treated with two or more drugs (Ickowicz, 2009, Tarride et al., 2006). However, [this]] does not imply that [neuropathic pain] patients with a higher number of analgesics are treated better (Schneider et al., 2020).
In fact, only 40–60% of patients have obtained sufficient pain relief with medications given in combination or alone (Dworkin et al., 2007). Surprisingly, one study stated that the universally used pregabalin and gabapentin are ineffective for most patients with neuropathic pain (Finnerup et al., 2015)."
Analysis of Mudunna et al's 2018 case study of three lactating women experiencing pain
In a 2018 US case series of three lactating women with nipple and/or breast pain, Mudunna et al assessed pain by using a cotton-bud and pin-prick touch, which the authors proposed were non-painful stimuli, moving from the lateral edge of each breast quadrant in towards the nipple. The women demonstrated heightened breast skin sensitivity to the stimuli.
Mudunna et al state
-
“Allodynia is perceiving a non-painful stimulus as painful. Other [breastfeeding] individuals experience increased pain from a normally painful stimulus (hyperalgesia). For a lactating woman with allodynia, an anatomically normal latch may be perceived as painful. Similarly, a woman with hyperalgesia may experience slight nipple compression during let down as excruciating.”
-
That in this descriptive case series of three, the women's pain resolved with oral antihistamines and beta-blockers. However, this very small study was unable to compare with the effects of the passage of time.
Fit and hold, and considerations of optimal biomechanics of infant suck, are omitted variable biases in this descriptive case series. That is, Mudunna et al do not attempt to clarify the mechanisms or indicators of an "anatomically normal latch" or "slight nipple compression during let down".
Mudunna et al also hypothesise that persistent local inflammation due to repetitive exposure to microtrauma is likely to sensitise the nociceptors and mechanoreceptors of nipple skin due to release of histamines and cytokines. Similarly, Mudanna et al hypothesise that an increased interstitial tension associated with the vasodilation and hypervascularity of breast inflammation triggers release of histamines and cytokines, sensitising surrounding tissues. These latter hypotheses align with the NDC mechanobiological model of nipple pain and damage.
Recommended resources
Persistent lactation-related nipple pain: aetiology and management
Are breastfeeding women more prone to persistent nipple pain if they have other skin conditions?
Selected references
Di Maio G, Villano I, Ilardi CR. Mechanisms of transmission and processing of pain: a narrative review. International Journal of Environmental Research and Public Health. 2023;20:3064 https://doi.org/3010.3390/ijerph20043064.
Amir LH, Jones LE, Buck ML. Nipple pain associated with breastfeeding: incorporating current neurophysiology into clinical reasoning. Aust Fam Physician 2015;44(3):127-32.
Berens P, Eglash A, Malloy M, et al. Persistent pain with breastfeeding: ABM clinical protocol #26. Breastfeeding Medicine 2016;11:46-56.
Brown A, Rance J, Bennett P. Understanding the relationship between breastfeeding and postnatal depression: the role of pain and physical difficulties. Journal of Advanced Nursing 2016;72(2):273-82.
Doshi TL, Dworkin RH, Polomano R. AAAPT diagnostic criteria for acute neuropathic pain. Pain Medicine. 2021;22(3):616-636.
Douglas PS, Geddes DB. Practice-based interpretation of ultrasound studies leads the way to less pharmaceutical and surgical intervention for breastfeeding babies and more effective clinical support. Midwifery 2018;58:145–55.
Douglas PS, Keogh R. Gestalt breastfeeding: helping mothers and infants optimise positional stability and intra-oral breast tissue volume for effective, pain-free milk transfer. Journal of Human Lactation 2017;33(3):509–18.
Douglas PS, Perrella SL, Geddes DT. A brief gestalt intervention changes ultrasound measures of tongue movement during breastfeeding: case series. BMC Pregnancy and Childbirth 2022;22(94):https://doi.org/10.1186/s12884-021-04363-7.
Fitzcharles M-A, Cohen SP, Clauw DJ, et al. Nociplastic pain: towards an understanding of prevalent pain conditions. The Lancet 2021;397:2098-110.
Garcia-Dominguez M. The role of TNF-alpha in neuropathic pain: an immunotherapeutic perspective. life. 2025;15(785):https://doi.org/10.3390/life15050785.
International Association for the Study of Pain. Definitions of chronic pain syndromes 2022 [Available from: https://www.iasp-pain.org/advocacy/definitions-of-chronic-pain-syndromes/.
International Association for the Study of Pain. Terminology 2022 [Available from: https://www.iasp-pain.org/resources/terminology/#pain.
Lucas R, Zhang Y, Walsh SJ, et al. OXTR rs53576 variation with breast and nipple pain in breastfeeding women. Pain Management Nursing 2021;22(3)
Mosely L. Reconceptualising pain according to modern pain science. Physical Therapy Reviews 2007;12(3):169-78.
Moseley LG, Butler DS. Fifteen years of Explaining Pain: the past, present, and future. The Journal of Pain 2015;16(9):807-13.
Muddana A, Asbill DT, Jerath MR, et al. Quantitative sensory testing, antihistamines, and beta-blockers for management of persistent breast pain: a case series. Breastfeeding Medicine 2018;13(4):275-80.
Odom E, Scanlon K, Perrine C, et al. Reasons for earlier than desired cessation of breastfeeding. Pediatics 2013;131:e726-32.
