Abscess: prevalence, presentation, pathophysiology, investigation
Definition
A lactation-related or puerperal abscess is an enclosed acute inflammatory mass which contains purulent debris.
Prevalence
Reported rates of lactational (puerperal) mastitis range from 2-20% of breastfeeding or lactating women.1 In recent Australia data the rate is at the higher end of the spectrum, at approximately 18%.2
One seminal Swedish study found that abscess occurred in about 3% of lactating women who present with a painful erythematous breast lump, regardless of whether or not antibiotics have been prescribed.3
Over the past 15 years, women have been advised to perform deep lump massage when they have mastitis, which results in microhaemorrhage and worsened inflammation in the sensitive and highly vascular tissue of an inflamed breast. This widespread practice isn't considered in prevalence estaimtes but may have caused iatrogenic increases in the rate of abscess formation.
You can find out about breast massage and lactation-related inflammation here.
Presentation
A lactational abscess presents as
-
A palpable beast mass with surrounding erythema, tenderness, +/- induration, or
-
Worsening deep breast pain with no superficial features and no palpable mass.
Here are the signs and symptoms of lactation-related breast inflammation when abscess is suspected, recorded using the NDC Classification of Benign Lactation-related Breast Inflammation.4 You can find out more about the NDC classification system here.
| Location of inflammation and pain | Dimensions (millimetres) | Erythema | Pain | Systemtic signs + symptoms |
|---|---|---|---|---|
| Generalised - bilateral | None | None | Feels well | |
| Generalised - unilateral | Mild | Mild when touched only | Fever | |
| Localised WITHOUT lump | Moderate | Mild constant | Myalgia | |
| Localised WITH lump | Severe | Moderate when touched only | Rigor | |
| Moderate constant | ||||
| Severe |
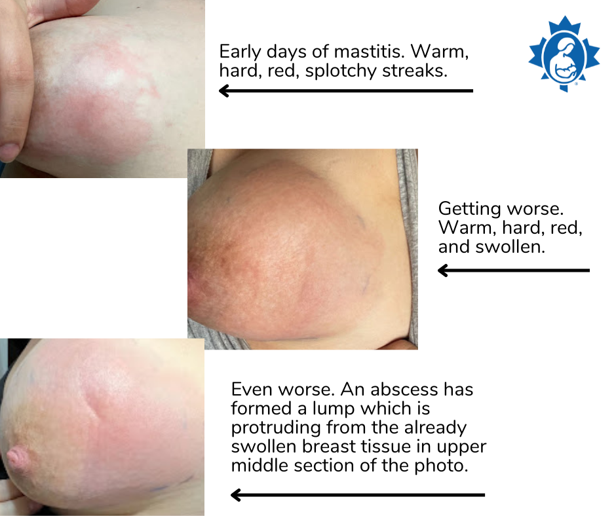
Image 1
Pathophysiology
Clinically, a lactational abscess is a localized collection of milk and purulent fluid, walled off by a stromal inflammatory reaction. The abscess also commonly has fibrotic septations in it. The contents of the abscess include
-
High white cell counts
-
Mammary epithelial cells
-
Bacteria and other microbiome microrganisms.
The NDC mechanobiological model of breast inflammation
The NDC mechnobiological model (here and here) hypothesizes that an abscess is an active end-stage inflammation (unilateral and localised), resulting from a focal area of alveolar rupture and inflammation.
According to the NDC model, intra-alveolar hydrostatic compression of the lactocytes results from either obstruction to outflow or from inadequate amounts of outflow. Resultant high intra-alveolar pressure causes rupture of the tight junctions between lactocytes, which results in rupture of the basement membrane, and involution of the alveolus. If these inflammatory processes become very highly activated or intense in a particular area of the stroma, involving many alveoli, clinically evident stromal connective tissue and lactiferous duct breakdown or necrosis ensues, associated with a collection of purulent fluid. The pus includes white cells, tissue debris, breast milk, and its microbiome.5-9
When this process occurs on a scale which is not been able to repair with tissue remodeling, the area remains in active inflammation and an abscess results.5
You can find out about the mechanobiological model of breast inflammation and its evidence-base here.
Indications for imaging
Ultrasound
Ultrasound imaging is the least invasive imaging option, and the most useful. It is indicated in a lactating woman for
-
Any breast lump that persists for more than a week, to exclude malignancy as well as abscess
-
An acutely inflamed breast lump which is growing in size or pain as the days progress, rather than gradually resolving with appropriate treatment as the days pass
-
Presentation of a breast lump with signs of fluctuant lump or signs of pointing
-
Deep and worsening or unresolved breast pain deep in the breast parenchyma, in the absence of a palpable breast lump.
The ultrasound features of an abscess include:
-
A well-circumscribed, irregular hypoechoic to heterogenous, typically multiloculated, lesion
-
No internval vascularity
-
Posterior acoustic enhancement from fluid
-
Echogenic, vascular rim (or thickened wall).10,11
Image 2
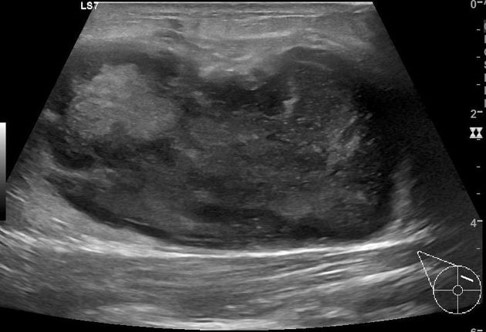
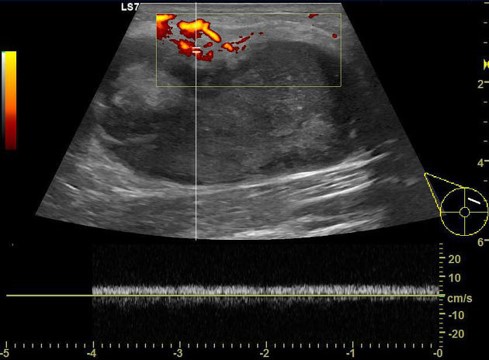
Image 3
Mammography
Mammography is not routinely indicated early on. The features of an abscess on mammography include asymmetric density, mass or distortion. Mammgraphy may be considered in a case of prolonged abscess in a woman older than 30 years of age. The clinician would wait until the acute phase has resolved before considering mammography.
Differential diagnoses
Ultrasound imaging of an inflamed breast lump may reveal
-
Lactation-related breast inflammation ('mastitis') only, discussed here
-
A phlegmon, discussed here, or
-
An abscess.
Other differential diagnoses, excluded by imaging, include
-
Malignancy
-
Inflammatory breast cancer
-
Ductal or lobula breast cancer
-
-
Phyllodes tumour.
You can find out about non-surgical management of lactational abscess here, fine needle aspiration (PAIR method) of lactational abscess here, and incision and drainage of lactational abscess here.
Acknowledgements
The breastfeeding art on this page is purchased from, and kindly used with consent by, Camilla Kleist at www.kleist-art.me.
Image 1: La Leche League Canada.
Images 2 and 3: Trop et al 2011 (12)
References
-
Wilson E, Woodd SL, Benova L. Incidence of and risk factors for lactational mastitis: a systematic review. Journal of Human Lactation. 2020;36(4):673-686.
-
Cullinane M, Amir LH, Donath SM, Garland SM, Tabrizi SN, Payne MS, et al. Determinants of mastitis in women in the CASTLE study: a cohort study. BMC Family Practice. 2015;16:181.
-
Kvist L, Larsson BW, Hall-Lord ML, Steen A, Schalen C. The role of bacteria in lactational mastitis and some considerations of the use of antibiotic treatment. International Breastfeeding Journal. 2008;3:6.
-
Douglas PS. Re-thinking benign inflammation of the lactating breast: classification, prevention, and management. Women's Health. 2022;18:17455057221091349.
-
Douglas P. Re-thinking benign inflammation of the lactating breast: a mechanobiological model. Women's Health. 2022;18:17455065221075907.
-
Jindal S, Narasimhan J, Vorges VF, Schedin P. Characterization of weaning-induced breast involution in women: implications for young women's breast cancer. Breast Cancer. 2020;6(55):https://doi.org/10.1038/s41523-41020-00196-41523.
-
Kobayashi K, Han L, Lu S-N, Ninomiya K, Isobe N, Nishimura T. Effects of hydrostatic ompression on milk production-related signaling pathways in mouse mammary epithelial cells. Experimental Cell Research. 2023;432:113762.
-
Stewart TA, Hughes K, Stevenson AJ, Marino N, Ju AL, Morehead M, et al. Mammary mechanobiology - investigating roles for mechanically activated ion channels in lactation and involution. Journal of Cell Science. 2021;134:doi:10.124/jcs.248849.
-
Weaver SR, Hernandez LL. Autocrine-paracrine regulation of the mammary gland. Journal of Dairy Science. 2016;99:842-53.
-
Febery, A. and I. Bennett, Sonographic features of inflammatory conditions of the breast. Australasian Journal of Ultrasound in Medicine, 2019. 22(3): p. 165-173.
-
Geddes DT. Ultrasound imaging of the lactating breast: methodology and application. International Breastfeeding Journal. 2009;4:doi:10.1186/1746-4358-1184-1184.
-
Trop I, et al. Breast Abscesses: Evidence-Based Algorithms for Diagnosis, Management, and Follow-Up. Radiographics. 2011;31(6):1683-99.
