The case of a breastfeeding mother who presented with exquisitely painful white spots on her nipple
Trish endures three months of very painful breastfeeding
This mother of a secondborn 15-week-old comes to see me having endured excruciating nipple pain whilst direct breastfeeding from her right breast. It started when the baby was about four weeks old. Since then, Trish has also consistently experienced deep stabbing or throbbing pain into the right breast between feeds, and painful, random bouts of vasospasm on the face of the right nipple (which didn't happen on the left). She tells me I am her last resort, her final hope for continued breastfeeding.
Amazingly, this woman's baby is thriving, contented, and gaining weight beautifully without supplementation. Despite the pain, she feeds her child from her right breast up to ten times over a 24-hour period (and similarly from the left). But she estimates that her left breast now produces perhaps four times more milk than the right. The baby tends to do a lot of pulling off the right breast.
A fortnight before Trish comes to see me, she'd had another white spot appear at about 2 o'clock on the face of her nipple, this time (and for the first time) with a wedge-shaped lump extending from her nipple up into the breast. Trish tells me that she'd lifted the roof of this new spot with her fingernail in the shower, which resulted in a spurt of milk and immediate easing of the painful lump in her breast.
Trish has done her research and has tried everything
Here are all the things this courageous woman has experimented with over the months since her baby's birth, in the hope that she would be able to continue breastfeeding.Her doctor had also organised breast imaging, which was normal. With the support of her general practitioner and an International Board Certified Lactation Consultant, she has tried
-
Keeping the nipple as moist as possible using olive oil between feeds
-
Unnroofing the white spots
-
Once by her doctor with bevelled needle, without benefit
-
Five times in the shower herself using a sterilised needle, without benefit. She has also pumped after the unroofing, having read that this would help clear the biofilm blockage. Pumping after using the needle resulted in multiple large clots of milk in the collecting bottle, which you can see in the photo below. Trish was of course worried that there had been so many clots with the pumping, fearing there was a worsening dysbiosis and biofilm inside her breast which she needed to pump out.
-
Regular gentle exfoliation of the white spots in the shower
-
-
Oral lecithin (ongoing) made from sunflowers
-
Many different approaches to fit and hold, including dangle feeding, football hold, cradle hold, and koala or straddle hold.
-
A course of the antibiotic cephalosporin
-
Regular use of the oral anti-inflammatory ibuprofen
-
Oral probiotics
-
Cold pack applications on the nipple and breast
-
Warm compresses on the nipple and breast
-
Use of the haaka to draw out the dysbiosis
-
Different kinds of breast massage
-
Allowing the nipple and breast to soak in a bowl of very warm water containing epsom salt
-
A course of the steroid cream triamcinolone acetonide 0.02%.
None of these interventions helped. They were time intensive and added a significant burden to Trish's days and nights. Although the treatments that she tried are popularly recommended, there is no evidence and also no plausible biological rationale to support the use of any of these treatments listed above. The exception is the trial of a steroid application, which has no evidence to support it's use but does have biological plausibility. It should not be used with a plastic wrap, which you sometimes hear recommended, due to the risk of moisture associated skin damage.
What is actually going on?
What are the relevant diagnoses?
Applying the NDC mechanobiological model of nipple pain, Trish's white spots are:
-
Hyperkeratosis of the right nipple, starting with a single white spot which developed into a line of hyperkeratosis horizontally across the face of the nipple.
-
A single milk blister two weeks ago. That is, the inflamed epithlium grew over a duct orifice or entrance on her nipple and resulted in a backup of milk in the area of the breast that drained into that duct.
What are the physiological or mechanical explanations?
Trish has experimented with fit and hold over the previous months, most commonly using a 'biological nurturing' (or koala or straddle hold) method of positioning the baby at her breast.
As I check out Trish's breast fall and breast-tummy contour, I also notice that her right nipple looks directly ahead or even slightly towards the midline. This is normal, but it does mean that she and her baby are at risk of the baby dragging the nipple and breast tissue too far towards the arm on the side from which she breastfeeds. It also makes it harder for her little one to have a slight backward tilt of her head and neck when breastfeeding.
This is why there has been so much consistent nipple and breast tissue drag, resulting from early on in repetitive microtrauma to the right nipple skin or epithelium. The high levels of focussed stretching forces on the nipple skin (which results from the nipple and breast tissue drag) have in her case caused horizontal hyperkeratosis across the face of her nipple, also associated with a wedging shape of the nipple when the baby comes off. The nipple and breast tissue drag has resulted in inflammation of the epidermis and a resultant thickening, like a callous. This is the body's way of attempting to protect the skin from the high and focussed stretching forces. Once a callous has formed, any pressure on it can result in tenderness or pain, the more so on a very sensitive part of the body like the nipple face.
Trish may also have inflammation of the deep nipple tissue from bending or deformational forces during breastfeeding. Most likely because of both of these effects, on the epidermis and also in the nipple stroma, she is experiencing acute pain with direct breastfeeding, and ongoing radiating inflammatory pain between breastfeeds.
Trish may have been predisposed to the milk blister a fortnight before she first sees me because of more general inflammatory processes on her right nipple epidermis. It's likely that there was an area of epidermal inflammation and epidermal disruption around a milk duct orifice. As it healed, the epithelium which runs a couple of millimetres into the milk duct from the entrance may have fused into an epidermal roof, causing a back up of milk into the branching duct system behind that specific orifice. This is a serious situation which requires your doctor to lift the roof. Or in truth, a lot of women in this situation soak the nipple epidermis with water in a warm shower then remove it themselves with their fingernail. The risk if you do this yourself is that it's not actually a milk blister, and you're accidentally worsening a hyperkeratosis! But a hyperkeratotic white spot, which is by far the more common, never has a true, painful build up of milk in the ducts behind it.
What I suggest Trish tries
We use the gestalt method and Trish feels immediate improvement in her pain levels during breastfeeding, from a six or seven usually, down to a two.
We then also try a size 24 nipple shield, which I am careful to fit with plenty of room (explaining to her why I did that). Trish tells me as the baby suckles after the nipple shield is on that her nipple pain is now down to a one. Although we kept trying with micromovements, we also know that we may not able to entirely eliminate pain today, even with the nipple shield, because of the pre-existing epithelial damage.
I advise Trish to allow her nipples to be exposed to the air as much as possible, at the same time as she continues a very active life outside the home. This is because overhydrated skin is much more vulnerable to mechanical injury during breastfeeding (or pumping). In particular, I recommend
-
Not using the olive oil
-
Sleeping without a bra at nights, using a towel to catch milk leakage.
-
Not allowing her damaged nipple to rub inside the breast pad, which may mean using protection such as a hydrogel disc, lanolin, or silverette when she does need to wear a bra.
I explain that lecithin, probiotics, and antibiotics won't help. We discuss trialling another course of steroid cream but Trish feels that the results with the gestalt method and nipple shield combination are so positive in the consultation (and there was no benefit from steroid when she tried it previously) that she wouldn't use a steroid application again for now.
I explain to Trish that
-
Hyperkeratosis is how the skin of her nipple attempts to protect her from high stretching forces. The epithelium thickens in response to repeated microtrauma.
-
Attempts to lift the roof of an area of hyperkeratosis and to exfoliate it unfortunately actually worsen the hyperkeratosis, because any abrasion or needle intervention worsens epithelial damage and the thickened protective response by the epithelium.
-
Two weeks ago, she'd had a milk blister, which is different to hyperkeratosis. I explain that Trish may have been predisposed to a milk blister because of general inflammation of the nipple epithelium, which can occasionally heal to seal over the entrance to a duct.
-
The clots resulted from the vacuum pressure of the pump being applied shortly after she'd lacerated the thickened area of hyperkeratosis. The pump kept drawing out blood from the epithelial laceration, not allowing the laceration to clot and stop bleeding. But as soon as blood mixes with milk, the tissue coagulation factors in milk turn the blood into clots. So there was nothing wrong inside her breast and nothing wrong with her milk.
-
The decreased milk production in the right breast despite such amazing effort to keep the baby on the right breast was likely due to poor milk transfer in the context of nipple and breast tissue drag, and an inevitable preferencing of longer feeds on the left breast in the context of so much pain on the right.
-
That a complete rest of the right breast would facilitate the quickest healing, with some hand expression to manage milk build up and prevent mastitis. Then she could start again on the right, this time with the gestalt method.
Trish decides to
-
Experiment with the gestalt method
-
Use the nipple shield on the right, still offering regularly
-
Keep her nipples as dry as possible, ensuring protection and safety of the right nipple as necessary.
I recommend review in a week, after a period of experimenting with the gestalt method, so that we can continue to work together as she experiments with this new approach.
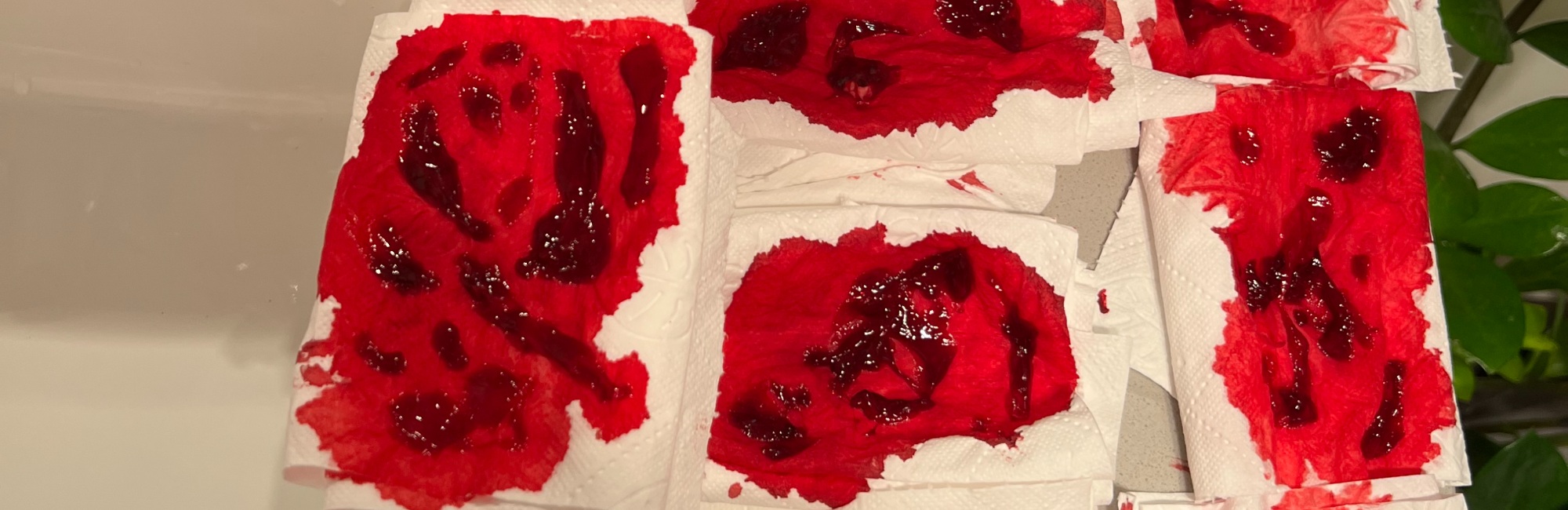
Here are photos Trish took of the frightening pumping session after she attempted to unroof the area of hyperkeratosis. I'm grateful to Trish for being willing to share them publicly (though her case is anonymised), in the hope of helping other breastfeeding women.
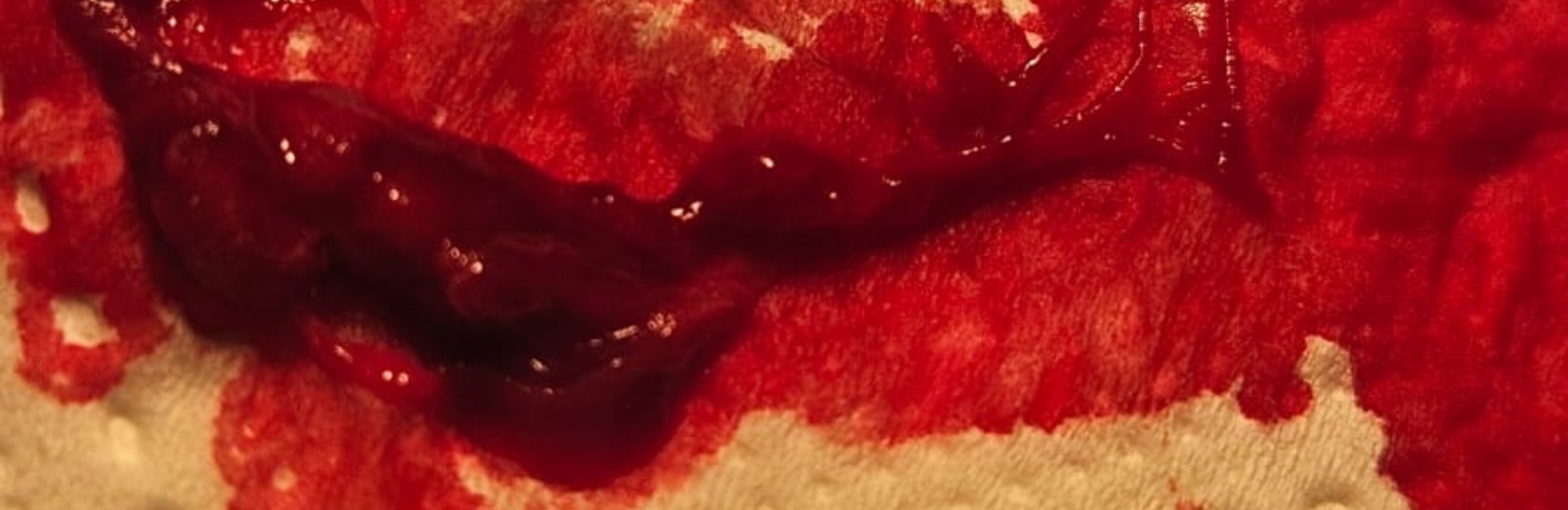
The blood clots were quite large. Trish was, of course, very worried when these clots seemed to keep coming out. She'd read that white spots were associated with dysbiosis and biofilm extending back into the breast (a theory widely publicised by the Academy of Breastfeeding Medicine's Clinical Protocol #36 which I contest in my 2022 research article in Women's Health on nipple pain and damage. I also critique the dysbiosis and biofilm theory of breast inflammation and white spots in a followup article I published in the International Breastfeeding Journal in 2023).

I explained that the mechanical pressure from the pumping kept freshening up the cut so that it continued to bleed, instead of clotting over as it normally would have. But at the same time as the cut kept freshening up, the blood from the cut mixed with human milk in the flange and bottle of the collecting system, and immediately clotted.
When Trish and her baby come back the following week not much has changed
The image below shows the hyperkeratotic white spots at this second consultation a week later, and how they hadn't reallly changed. The photo at the top of this page is from the initial consultation.
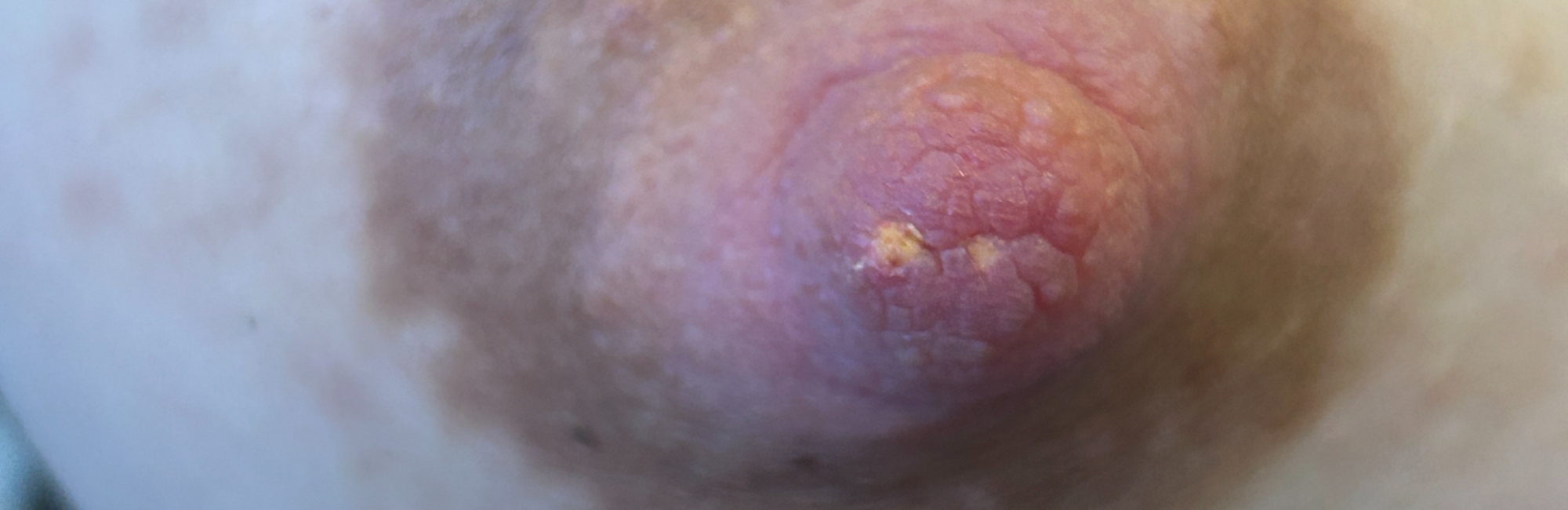
The next image below shows these white spots hydrated by the milk and baby's saliva, and made prominent in response to the vacuum pressures, after Trish had put baby to her right breast during that second consultation.

Unfortunately, not much has changed a week later, when we meet again. The nipple shield hasn't worked because the baby kept knocking it off or it kept slipping off, and for Trish the shield just seemed to make everything harder rather than easier. I completely understand this, though I do mention that there are tricks for dealing with these challenges with the shield, which are common at first.
I suggest that one option is to keep on trying the shield every now and then, because in my view it still offers the possibility of protecting the white spots from the mechanical pressures. But I can also see how important it is not to put any pressure on Trish, who really is at the end of what has been a very long and distressing road of pain.
Trish had been experimenting bravely with the gestalt method on the right (but found it easiest to continue with her usual straddle hold on the left, which had always worked well for her and the baby on that side). It can be difficult making changes once a baby is four months old, as a baby becomes used to a certain way of doing things! Despite trying, Trish hadn't been able to achieve the same decrease in pain that she'd experienced in our initial consultation together. Again, this is quite commonly the case, and I find it can take a couple of sessions working together on fit and hold to turn the corner when a woman has nipple pain. I can see when she breastfeeds this time that the baby is still feeding too far off to the side, relative to the location of her right nipple. We work together on the gestalt method again.
Trish is discouraged, though, by the lack of progress, and demoralised by the constaint pain. Just that morning, she explains, she had a bout of vasospasm on the right, in between breastfeeds, which caused pain for about two hours.
We discuss in greater detail the options that are available to her. I explain how healing up a hyperkeratosis of the nipple can take weeks, how it is like waiting for a callous to be absorbed by the body once the repetitive mechanical pressures which cause it have ceased or eased. But Trish is seriously exhausted by the ongoing pain, and considering either weaning, or at least resting the right breast and introducing some commercial milk formula to compensate. We discuss various options in depth, knowing that there is no right or wrong path forward concerning the use of commercial milk formula. There is only the consideration of what Trish can now manage, as she weighs up the importance of enjoying her days and nights with her baby after so many months of trying to change the pain. All the while, I communicate my view that she's been extraordinarily courageous in the face of severe difficulty, and that it's important to celebrate the way she's given her baby a whole four months of amazing gut and immune protection, despite everything.
When we say goodbye, we decide not to make a followup appointment, as Trish feels she now has the tools she needs, and is ready to find her own path forward now, day by day.
Two weeks later, Trish is preparing to wean
Trish communicates to me a couple of weeks later that whilst her baby continues to thrive, her hyperkeratotic spots haven't changed, and if anything the pain is worse. She has also had another milk blister, in exactly the same place. Trish says that she is now preparing to wean, trying to build a stash of expressed breast milk in the freezer before she does so.
I agree that only completely stopping the application of a vacuum to her right breast (by weaning and stopping pumping on the right) will allow these entrenched hyperkeratotic spots to heal. This may take weeks, the way it takes callouses weeks to absorb. I can't help but wonder, in my own mind, how breastfeeding would have gone for Trish if she'd received effective help very early on to eliminate nipple and breast tissue drag, along with advice not to disrupt the skin of her nipple with unroofing, exfoliations, and moist applications. I believe Trish would have had a much greater chance of healing without needing stop breastfeeding and pumping.
This story is blended from multiple presentations of nipple white spots during lactation that I've been and no individual patient is able to be identified from this story.
Recommended resources
Nipple white spot during breastfeeding #1: hyperkeratosis
Nipple white spot during breastfeeding #2: epidermal inclusion cyst
Nipple white spot during breastfeeding #3: milk blister
Selected references
Douglas PS. Re-thinking lactation-related nipple pain and damage. Women's Health. 2022;18:17455057221087865.
Douglas PS. Does the Academy of Breastfeeding Medicine Clinical Protocol #36 'The Mastitis Spectrum' promote overtreatment and risk worsened outcomes for breastfeeding families? Commentary. International Breastfeeding Journal. 2023;18:Article no. 51 https://doi.org/10.1186/s13006-13023-00588-13008.
Hu Y, Hell L, Kendibacher RA. Human milk triggers coagulation via tissue factor–exposing extracellular vesicles. Blood Advances. 2020;4(24):6274-6282.
